Obinwanne Chukwuemeka Junior (OD, FAAO, FLVPEI, FSLS)
Head Of Cornea, Specialty Contact Lenses and Myopia Control Services, De Lens Ophthalmics Family Eye and Vision Care Centre, Febson Mall, Abuja, Nigeria.
Vernal keratoconjunctivitis (VKC) is a chronic form of ocular allergic disease of the cornea and conjunctiva and presents with common symptoms like severe itching, redness, tearing, grittiness and pain.
The etiology of VKC is multifactorial. However, the increased levels of IgE in the tear film plays a pivotal role in its occurrence. VKC is a type 1 hypersensitivity reaction with Th2 lymphocytes acting as mediators, activating basophils and eosinophils, leading to mast cell degradation and a subsequent release of histamines. The itchy sensation and conjunctival redness seen in this disease result from these reactions. Typically, there are three variants of VKC: the palpebral variant, limbal variant and the mixed variant.
Clinical signs in VKC are typically present on both the cornea and conjunctiva. The disease presentation depends on the variant. Still, certain classical signs may present in all three variants.
- Papillae on the upper palpebral conjunctiva
- Stringy mucous discharge
- Bulbar conjunctiva redness
- Perilimbal pigmentation
- Muddy appearance of the conjunctiva
The signs and presentation of VKC are essential for their classification. The palpebral variant is characterized by upper tarsal conjunctiva giant papillae but without cornea involvement. Limbal VKC presents with cornea epithelial disease, limbal thickening and gelatinous appearance of the limbus, Horner-Trantas dots (limbal papillae), cornea erosion and shield ulcers. The mixed variant, which is by far the most common, is a combination of the palpebral and limbal variants.
VKC patients characteristically report severe itching, blurry vision, foreign body sensation, blepharospasm, red and puffy eyes, ropy discharge and high sensitivity to light. These signs and symptoms form the basis on which the severity of VKCs is graded. Gokhale recently proposed a severity grading system that considers the patient’s symptoms and signs.[1]
The grades are mild, moderate-intermittent, moderate-chronic, severe and blinding (Table 1). The grading system is done per eye and should be repeated at each visit to the clinic. Though uncommon, VKC can indeed lead to blindness.[2]
| MILD | MODERATE-INTERMITTENT | MODERATE-CHRONIC | SEVERE | BLINDING |
| Symptoms and papillae | Findings from mild stage + Trantas dot, <6 clock hours of limbal inflammation and puncate cornea erosions | Findings from mild and moderate intermittent stage + cobblestone papillae | Findings from mild and moderate stage + >6 clock hours of limbal inflammation, coarse SPKs, conjunctival granulomas, LSCD-pannus, macro-erosions. | Findings from severe stage + shield ulcers, LSCD with conjunctivalization and vascularization. |
Table1: Grading the severity of vernal keratoconjunctivitis
(Adapted from: Gokhale NS. Systematic approach to managing vernal keratoconjunctivitis in clinical practice: Severity grading system and a treatment algorithm. Indian J Ophthalmol. 2016 Feb;64(2):145-8. doi: 10.4103/0301-4738.179727. PMID: 27050351; PMCID: PMC4850811).
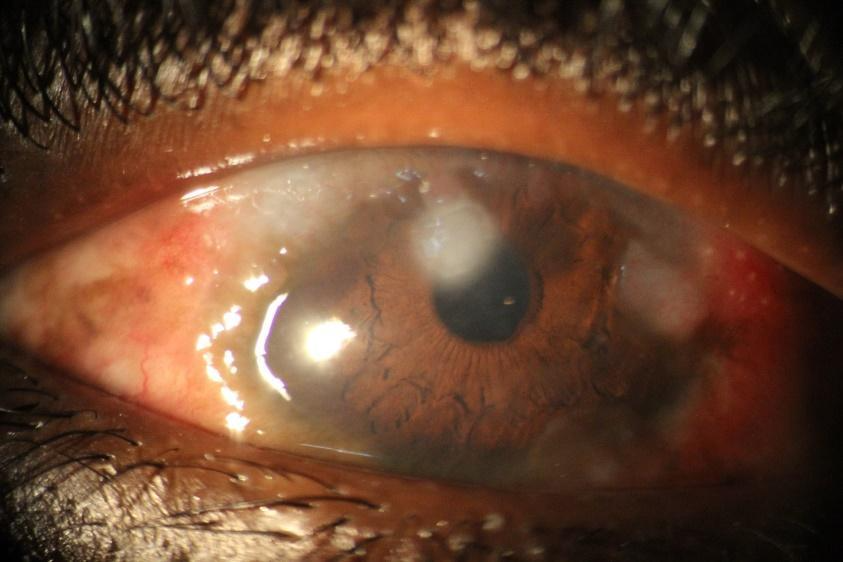
Image 1: Severe VKC with shield ulcer, Horner-Trantas dots, limbal thickening and vascularization in a teen.
Complications seen in VKC patients include punctate keratopathy, limbal stem cell deficiency, shield ulcers, pseudogerontoxon, dry eye disease from the cornea complication, keratoconus from cornea thinning due to mechanical eye rubbing and microbial keratitis secondary to epithelial compromise and long term topical steroid use.
MANAGEMENT PEARLS
Mast Cell Stabilizers and Antihistamines
Mast cell stabilizers are regarded as the first line of management in non-limbal vernal keratoconjunctivitis cases. These agents, especially the newer generation ones, prevent the degranulation of mast cells and also act against eosinophils, neutrophils, and macrophages. These properties make their use appropriate in some cases of VKC with cornea involvement, such as VKC with keratitis and shield ulcers. However, lodoxamine appears to be superior in this regard.[3]
Anti-histamines may also be employed in mild cases — these agents are H1 receptor antagonists and help mitigate histamine action. They relieve symptoms of itching and redness and are potent in seasonal cases. Newer generations have a longer duration of action and do not sting as the older ones did. Some combine mast cell stabilizing properties with anti-histamine properties and have a rapid onset of action; examples include Olopatadine and Ketotifen.
Corticosteroids
Topical corticosteroids are commonly prescribed in the management of VKC. They quell inflammation by preventing the recruitment of inflammatory mediators involved in the cascade of vernal keratoconjunctivitis etiology.
Cornea involvement and giant papillae on the upper tarsal conjunctiva are indications for steroid use. Considering the risk of blinding corneal complications, the benefits of using topical steroids mostly outweigh the risks. Steroid use must always be done with caution. Pay attention to intraocular pressures and crystalline lens clarity; review children every two weeks and screen for cataracts and secondary intraocular pressure rise.[4]
The potential of microbial keratitis should also be considered, especially when the cornea epithelium is compromised, as in punctate keratopathy or shield ulcers. Milder steroids such as Fluorometholone and Loteprednol are advocated. The clinician may move to more potent steroids, sub-tarsal steroid injections or oral steroids when milder ones prove ineffective.
Tacrolimus
Tacrolimus, a calcineurin inhibitor that prevents T-lymphocyte activation, and has shown to be efficacious in refractory cases of vernal keratoconjunctivitis.[5] Clinical signs and symptoms were shown to resolve in 4 weeks, and giant papillae resolved in 8 weeks. Patients only required tear substitute drops while on tacrolimus. One major adverse event of this medication is the stinging sensation on instillation. The ointment preparation and dermatologic grade of Tacrolimus are also efficacious in managing refractory VKC.
Cyclosporine
Oral and topical cyclosporine are also credible options in treating refractory VKC, mainly in cases involving shield ulcers or where the side effects from corticosteroids are being avoided. Cyclosporine inhibits the proliferation of Th2 lymphocytes and interleukin production. It has been shown to decrease histamine release as well as eosinophils and basophils. Through this mechanism, they have been shown effective in managing VKC. Just like with tacrolimus, some patients experience burning on instillation.
Adjunct Therapies
Medically Necessary Contact Lens
Bandage contact or scleral lenses may be used with other pharmacologic treatments for managing severe ocular surface disease associated with VKC. These scenarios include shield ulcers and severe epithelial erosion. The lenses protect the fragile cornea from further weathering and mechanical interaction with the palpebral conjunctiva. In cases where irregular astigmatism or keratoconus is present, scleral lenses can be used for visual rehabilitation.
Lubricants
Though lubricating drops are not directly used in managing VKC, they are essential in providing symptomatic relief to patients with VKC. They decrease symptoms of dryness, improve ocular surface epitheliopathy and dilute inflammatory mediators on the ocular surface.
Visual Rehabilitation
VKC is commonly seen in children who instinctively rub their eyes when it itches. As a result of the constant rubs, they often present with astigmatism, may have amblyopia and can develop keratoconus. It is important that refraction, keratometry and/or corneal topography be done once the ocular surface is stable. The appropriate corrective measure be it spectacles or specialty contact lenses, should be initiated in time, with the ocular surface and strict hygiene in mind.
REFERENCES
- Gokhale NS. Systematic approach to managing vernal keratoconjunctivitis in clinical practice: Severity grading system and a treatment algorithm. Indian J Ophthalmol. 2016 Feb;64(2):145-8. doi: 10.4103/0301-4738.179727. PMID: 27050351; PMCID: PMC4850811.
- Al-Akily SA, Bamashmus MA. Ocular complications of severe vernal keratoconjunctivitis (VKC) in Yemen. Saudi J Ophthalmol. 2011 Jul;25(3):291-4. doi: 10.1016/j.sjopt.2011.02.001. Epub 2011 Feb 16. PMID: 23960939; PMCID: PMC3729521.
- Mantelli, F., Santos, M. S., Petitti, T., Sgrulletta, R., Cortes, M., Lambiase, A., & Bonini, S. (2007). Systematic review and meta-analysis of randomised clinical trials on topical treatments for vernal keratoconjunctivitis. The British journal of ophthalmology, 91(12), 1656–1661. https://doi.org/10.1136/bjo.2007.122044
- Sen, P., Jain, S., Mohan, A., Shah, C., Sen, A., & Jain, E. (2019). Pattern of steroid misuse in vernal keratoconjunctivitis resulting in steroid induced glaucoma and visual disability in Indian rural population: An important public health problem in pediatric age group. Indian journal of ophthalmology, 67(10), 1650–1655. https://doi.org/10.4103/ijo.IJO_2143_18.
- Fiorentini SF, Khurram D. Therapeutic effects of topical 0.03% Tacrolimus ointment in children with refractory vernal keratoconjunctivitis in Middle East. Saudi J Ophthalmol. 2019 Apr-Jun;33(2):117-120. doi: 10.1016/j.sjopt.2019.04.001. Epub 2019 May 17. PMID: 31384152; PMCID: PMC6664310.