Often, the patient with keratoconus has seen several doctors before landing on your chair. They are anxious, wondering if this consultation will be any different from others, worried about the continuous visual decline from a condition with such a funny name and the huge impact on their quality of life.
Several options abound for visual rehabilitation of the patient with keratoconus, non-surgical and surgical. The typical consultation for the patient with keratoconus goes from history, ocular examination, corneal tomography, visual rehabilitation with specialty contact lenses or surgical intervention or a combination of both. However, as eye care practitioners managing keratoconus, we do not always remember or talk about the psychological impact the disease has on the PERSON suffering the condition.
Several studies have shown depression1, and increased neuroticism2 in patients with keratoconus and these psychological disorders worsen with worsening of vision3. In spite of ample evidence pointing to the impact of keratoconus on the mental health of patients, basic assessment to detect psychological disorders is not yet standard of care. Depression is associated with increase in suicidal attempts and mortality 4 and early detection of the disorder may prevent further deterioration in mental health and improve quality of life.
Visual rehabilitation, especially with scleral lenses improves vision as well as quality of life in patients with keratoconus5, however, difficulty handling the lenses may lead to drop out and one study even showed higher depression in patients who wore specialty lenses in both eyes compared to patients with unilateral disease1. While this may seem surprising, but a deeper look at the results indicates that patients with more severe, bilateral disease may still remain depressed even after being corrected visually. This may stem from difficulty handling lenses, fear of losing lenses, inability to afford lenses or other services or management options required for management of the disease, and complications associated with advanced keratoconus such as cornea hydrops.
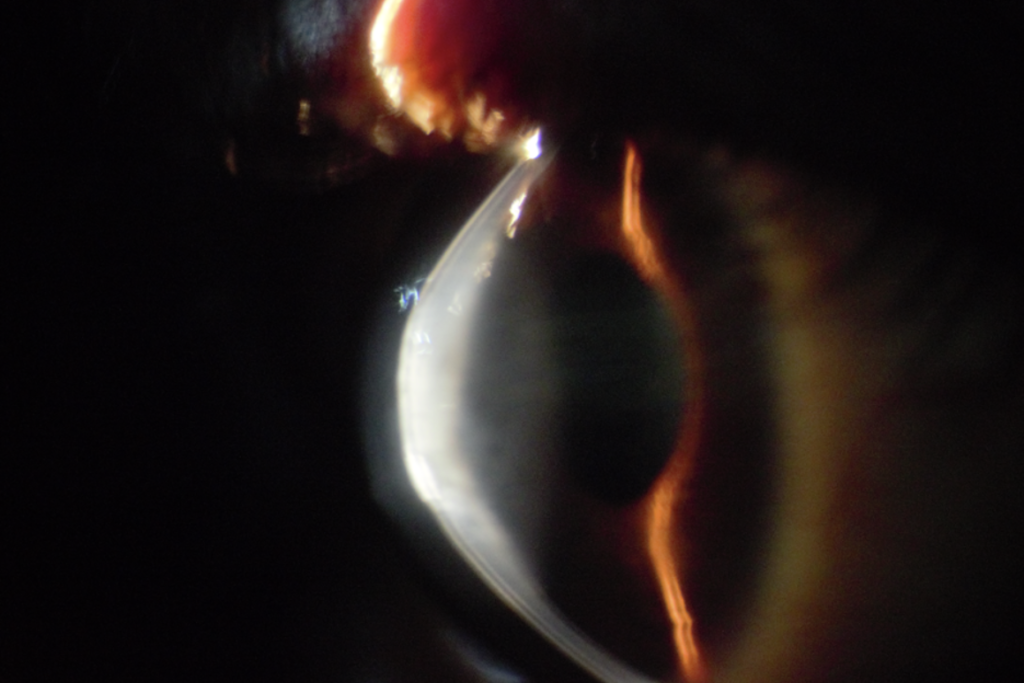
The impact of keratoconus on the mental health of individuals with the disease is unknown in Africa, and sadly severe complications such as hydrops (Figure 1) and severe visual impairment can occur in childhood. I recall a patient explaining the anxiety she feels when handling her lenses for fear of breaking them, keeping in mind the cost of the lenses, no insurance cover, risk of infections and other issues which may come with the lenses. This may not be peculiar to Africa alone as patients with lower socioeconomic status irrespective of where they are may suffer similar circumstances. These burdens may plague the mind of a patient with keratoconus and their quality of life.
Our cutting-edge lenses and surgical techniques are great, but the next time we encounter a patient with keratoconus, the onus is upon us to spend a few minutes talking to the person and not just treating the cornea disease. Ask questions about the impact of the disease on their quality of life and how best to help them. For children affected with the disease, parents, care givers and teachers should understand the condition and its impact on their quality of life and mental health. Steps should be put in place to ensure the child’s life is not impacted by the disease as much possible. Have a general practitioner, psychologist or psychiatrist as part of your referral team and make prompt referrals when indicated. Stock up on questionnaire such as the PHQ-9 questionnaire, which is an instrument for screening, diagnosing and even monitoring depression6.
We may not solve all the issues facing the patient with keratoconus, but we can certainly ensure that the person suffering the disease is cared for as a person and their wellbeing beyond visual improvement is taken care of.
REFERENCES
- Al-Dairi W, Al Sowayigh OM, Al Saeed AA, Alsaad A. Depression Among Keratoconus Patients in Saudi Arabia. Cureus. 2020 Dec 6;12(12):e11932. doi: 10.7759/cureus.11932. PMID: 33425513; PMCID: PMC7785487.
- Aslan MG, Besenek M, Akgoz H, Satılmaz MF, Hocaoglu C. Evaluation of Personality Features and Mental State of Keratoconus Patients. Beyoglu Eye J. 2021 Dec 17;6(4):272-279. doi: 10.14744/bej.2021.24482. PMID: 35059573; PMCID: PMC8759553.
- Moschos MM, Gouliopoulos NS, Kalogeropoulos C, Androudi S, Kitsos G, Ladas D, Tsatsos M, Chatziralli I. Psychological Aspects and Depression in Patients with Symptomatic Keratoconus. J Ophthalmol. 2018 May 29;2018:7314308. doi: 10.1155/2018/7314308. PMID: 30002924; PMCID: PMC5996428.
- (Abate K. H. (2013). Gender disparity in prevalence of depression among patient population: a systematic review. Ethiopian journal of health sciences, 23(3), 283–288. https://doi.org/10.4314/ejhs.v23i3.11
- (Kreps, E. O., Pesudovs, K., Claerhout, I., & Koppen, C. (2021). Mini-Scleral Lenses Improve Vision-Related Quality of Life in Keratoconus. Cornea, 40(7), 859–864. https://doi.org/10.1097/ICO.0000000000002518.
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606-13. doi: 10.1046/j.1525-1497.2001.016009606.x. PMID: 11556941; PMCID: PMC1495268.