Despite the significant advancements and investments in creating more comfortable contact lenses, the number of people who wear them has not significantly increased worldwide. Researchers have attempted to understand the etiology of contact lens discomfort to develop effective management strategies. However, it is crucial to differentiate between discomfort and dry eye disease caused by contact lenses.
The Tear Film Ocular Surface Society (TFOS), in its workshop on contact lens discomfort, defines contact lens discomfort as “a condition characterized by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment, which can lead to decreased wearing time and discontinuation of contact lens wear.”[1]
On the other hand, contact lens wearers may experience dry eye disease, which can either be induced (known as contact lens-induced dry eye disease or CLIDE) or associated (known as contact lens-associated dry eye disease). The difference lies in the absence of pre-existing dry eye disease before the initiation of contact lens wear (CLIDE)[2] According to a significant population-based study, dryness in contact lenses can impact up to 50% of wearers.[3] It is crucial to address this concern to enhance the comfort of contact lens wearers, drive growth in the industry, and achieve clinical success in patient management.
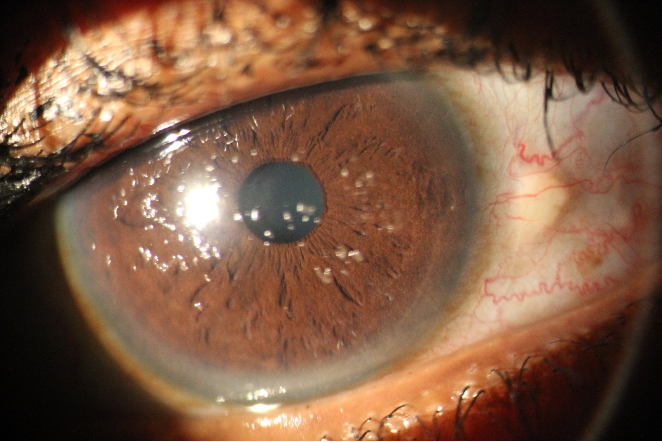
Inserting a contact lens into an eye affects the tear film, causing it to split into pre and post-contact lens tear film. The composition and stability of the pre-lens tear film differ from that of an eye without contact lenses. This can lead to dryness and discomfort as there is no mucous layer on the contact lens surface, increased friction between the tarsal conjunctiva and the contact lens surface, and changes in the lipid layer of tears.
The type of contact lens material used also contributes to the development of dryness and affects overall comfort. While artificial tear drops are commonly used to manage dryness in contact lens wearers, specific properties of the contact lens, such as its water content, play a crucial role in developing CL-related dryness.
Research has shown that low-water-content contact lenses are less likely to cause dry eye symptoms compared to high-water-content lenses. Individuals wearing FDA group 2 contact lenses (high-water-content and non-ionic lenses) are more prone to experiencing dry eyes than those who wear FDA group 1 contact lens materials (low water content and non-ionic lenses).[5]
High water content contact lens wear has been associated with dry eye disease, even when age and gender are considered.[6] The reasons for this association include increased evaporation, deposit formation, and changes to the surface of the lens in high water content lenses.[5] These factors can affect the lens’ ability to transmit oxygen, flexibility, movement, and other properties.[7]
| FDA Group | Water content | Ionicity |
| I (examples Polymacon, Lotrafilcon A&B) | Low water content | Non ionic |
| II ( Omafilcon A, Hilafilcon A) | High water content | Non-ionic |
| III (Balafilcon A) | Low water content | Ionic |
| IV (Etafilcon A, Ocufilcon D) | High water content | Ionic |
Table 1: FDA classification of soft contact lens materials based on water content and surface ionicity with some common material examples.
Another potential cause of dryness while wearing contact lenses is pervaporation. This happens when water from the tear film beneath the lens seeps into the lens material and evaporates. This can result in feeling of dryness, and in some cases, the lens may adhere to the cornea epithelial surface. Pervaporation is more common with high water content and silicon lenses.
The wettability of a contact lens is crucial in causing dryness. Contact lenses treated with surfactants or having lower wetting angles exhibit better wetness and lesser dryness than untreated ones. In laboratories, wettability is measured by the contact angle of a liquid drop with the lens surface, where a lower angle indicates better surface wetness. Clinically, this can be checked while the patient blinks with the lens on, by assessing the tear breakup under a slit lamp biomicroscope. Poor wetting lenses tend to break tears quickly. It is also known that lens care solutions can affect surface wetness and deposit formation, with hydrogen peroxide-based solutions performing better than multipurpose-based ones.[8]
The material properties, water content, and surface ionic charge can contribute to the formation of deposits on contact lenses. Studies have shown that lenses in FDA group 4 (high water content and ionic) tend to have more protein deposition. In contrast, those in FDA group 2 (high water content, non-ionic) are more susceptible to lipid deposition.[9] These deposits may trigger low grade inflammatory responses to the ocular surface leading to contact lens induced papillary conjunctivitis and worsen the dry eye symptoms.
There has been conflicting results on the impact of silicone hydrogel contact lenses on dry eyes and comfort. Nevertheless, these lenses have demonstrated enhanced comfort in certain studies compared to hydrogel lenses. This is attributed to their superior oxygen transmissibility, surface wettability, reduced deposit formation, and lower evaporation levels.[5]
Contact lens wearers who have lid wiper epitheliopathy and conjunctival chalasis may experience more severe dry eye symptoms compared to those without these ocular surface disease characteristics.[4] In addition, other factors such as contact lens thickness, poor blinking patterns, co-existing meibomian gland dysfunction, and environmental conditions can also contribute to dryness during contact lens wear.
Management
Asides management of pre-existing ocular surface disease, enhancing the wettability of the lens and increasing the thickness of the tear film in front and around of the contact lenses are ways dryness in contact lenses can be addressed. One way to achieve this is by using disinfecting solutions containing lubricating agents. Also, studies have shown that soaking the lenses in lubricating solutions before insertion can improve initial comfort, wettability and decrease discomfort. Switching to peroxide-based solutions can protect against dryness and punctate cornea erosion caused by preservatives in other solutions, which can impact overall comfort.
For patients who use daily wear contact lenses, it is worth considering the switch to daily disposables. By replacing them more frequently, deposit build-up can be reduced, leading to less discomfort and decreased dryness symptoms.
Consider moving patients to lower water content lenses when they experience dryness with high water content lenses. Choose lens materials with lubricating or surfactant-wetting agents embedded in the lens material matrix to decrease evaporation and dryness. Opting for third-generation silicone hydrogels, which are naturally wettable materials, can also improve lens wettability and alleviate dryness.
As always, the use of topical lubricating drops has shown to improve symptoms and signs of dryness and improved comfort. Avoid the use of artificial tears with preservatives during contact lens wear as the contact lens may act as a sponge and slowly release these preservatives to the ocular surface; they harm the ocular surface and exacerbate dry eyes. Managing existing ocular surface disease like meibomian gland dysfunction or lid abnormalities, is advised, as this is paramount in achieving overall clear and comfortable contact lens wear.
REFERENCES
- Nichols JJ, Willcox MD, Bron AJ, Belmonte C, Ciolino JB, Craig JP, Dogru M, Foulks GN, Jones L, Nelson JD, Nichols KK, Purslow C, Schaumberg DA, Stapleton F, Sullivan DA; members of the TFOS International Workshop on Contact Lens Discomfort. The TFOS International Workshop on Contact Lens Discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013 Oct 18;54(11): TFOS7-TFOS13. doi: 10.1167/iovs.13-13212. PMID: 24058135; PMCID: PMC4686219.)
- Gomes, J. A. P., Azar, D. T., Baudouin, C., Efron, N., Hirayama, M., Horwath-Winter, J., Kim, T., Mehta, J. S., Messmer, E. M., Pepose, J. S., Sangwan, V. S., Weiner, A. L., Wilson, S. E., & Wolffsohn, J. S. (2017). TFOS DEWS II iatrogenic report. The ocular surface, 15(3), 511–538. https://doi.org/10.1016/j.jtos.2017.05.004.
- Dumbleton, K., Caffery, B., Dogru, M., Hickson-Curran, S., Kern, J., Kojima, T., Morgan, P. B., Purslow, C., Robertson, D. M., Nelson, J. D., & members of the TFOS International Workshop on Contact Lens Discomfort (2013). The TFOS International Workshop on Contact Lens Discomfort: report of the subcommittee on epidemiology. Investigative ophthalmology & visual science, 54(11), TFOS20–TFOS36. https://doi.org/10.1167/iovs.13-13125.
- Stapleton, F., & Tan, J. (2017). Impact of Contact Lens Material, Design, and Fitting on Discomfort. Eye & contact lens, 43(1), 32–39. https://doi.org/10.1097/ICL.0000000000000318// Nichols, J. J., & Sinnott, L. T. (2006). Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Investigative ophthalmology & visual science, 47(4), 1319–1328. https://doi.org/10.1167/iovs.05-1392.
- Ramamoorthy P, Sinnott LT, Nichols JJ. Treatment, material, care, and patient-related factors in contact lens-related dry eye. Optom Vis Sci. 2008 Aug;85(8):764-72. doi: 10.1097/OPX.0b013e318181a91f. PMID: 18677240; PMCID: PMC2628947.
- Nichols, J. J., & Sinnott, L. T. (2006). Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Investigative ophthalmology & visual science, 47(4), 1319–1328. https://doi.org/10.1167/iovs.05-1392.
- Tranoudis I, Efron N. Parameter stability of soft contact lenses made from different materials. Cont Lens Anterior Eye 2004;27:115-31.
- Guillon, M., Maissa, C., Wong, S., Patel, T., & Garofalo, R. (2015). Effect of lens care system on silicone hydrogel contact lens wettability. Contact lens & anterior eye: the journal of the British Contact Lens Association, 38(6), 435–441. https://doi.org/10.1016/j.clae.2015.06.007.
- Jones, L., Evans, K., Sariri, R., Franklin, V., & Tighe, B. (1997). Lipid and protein deposition of N-vinyl pyrrolidone-containing group II and group IV frequent replacement contact lenses. The CLAO journal: official publication of the Contact Lens Association of Ophthalmologists, Inc, 23(2), 122–126.